Atrial Fibrillation: Medical Therapy or Ablation?
By Brian D. Powell, MD, FACC, FHRS
Medical Director of Cardiac Electrophysiology
Sanger Heart & Vascular Institute
Atrial fibrillation is the most common arrhythmia and is associated with significant morbidity and mortality. Catheter ablation is increasingly being used to treat atrial fibrillation, but how do you know if it's right for your patient? Asking these questions can help you make the right choice.
Is my patient symptomatic?
Patients with atrial fibrillation who have little or no symptoms can often be managed with a rate control and anticoagulation strategy. If their symptoms are controlled, and heart rates can be kept under 110 bpm, rate control is a reasonable strategy. In contrast, patients with moderate or severe symptoms from atrial fibrillation, or difficult rate control, can benefit from a strategy of trying to maintain sinus rhythm with either antiarrhythmic drug therapy or ablation.
Should my patient try an antiarrhythmic drug before considering ablation?
In general, yes. Guidelines recommend trying an antiarrhythmic drug first in most patients. However, there is an exception. Patients who have lone, paroxysmal atrial fibrillation with no significant comorbidities and a normal or mildly enlarged left atrium should consider an earlier ablation strategy. Those patients have the highest chance for success with ablation.
How is atrial fibrillation ablation performed?
The primary approach to atrial fibrillation ablation is to isolate the pulmonary veins. This can be done with either radiofrequency ablation (heat energy) or cryoablation (freezing balloon). Additional ablation is performed if atrial fibrillation remains refractory in spite of pulmonary vein isolation, or if atrial flutters are induced.
How successful is atrial fibrillation ablation?
Multicenter trials have reported one-year success rates free from atrial fibrillation of approximately 80 percent for paroxysmal atrial fibrillation (atrial fibrillation that occurs occasionally), and approximately 70 percent for persistent atrial fibrillation (atrial fibrillation lasting >7 days or requiring cardioversion).
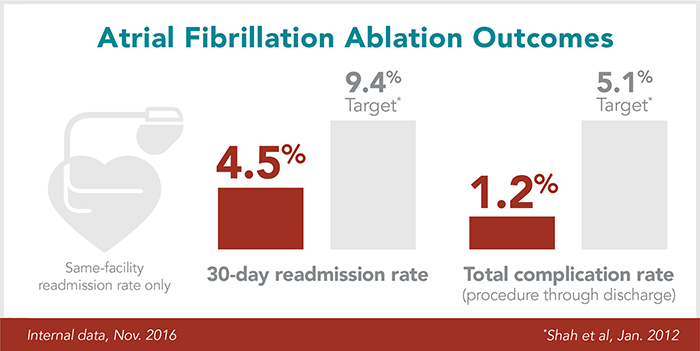
Sanger Heart & Vascular Institute consistently achieves top outcomes, with ablation readmission rates that are half the national average and complication rates that are 75 percent lower than what’s reported in multicenter registries.
What happens to patients with recurrent atrial fibrillation after an ablation procedure?
At Sanger, we use antiarrhythmic drugs during the first 3 months post-ablation to treat symptomatic arrhythmias. During that time, the atrium is inflamed. Time is required for that inflammation to transition to lines of scar tissue around the pulmonary veins to maintain electrical isolation and avoid pro-arrhythmia from the inflammation. If atrial fibrillation continues beyond 3 months post-ablation, options include a second ablation procedure or continuing antiarrhythmic drug therapy if that has been effective and tolerated.
What if my patient has complex arrhythmias?
Mapping systems have improved to allow for more rapid and detailed mapping of atypical atrial flutters that can occur after an initial ablation procedure. Sanger Heart & Vascular Institute electrophysiologists work with the most advanced 3D mapping systems and are experienced with patients referred for repeat ablation procedures after an initial attempt at ablation.
Atypical atrial flutters can often be mapped and targeted for ablation with either additional linear ablation connecting nonconducting structures, or focal ablation for microreentrant arrhythmias. The success rate improves to approximately 85 percent when allowing for more than one ablation procedure.
Want to know more? Connect with one of our electrophysiologists by calling 704-373-0212.
